Abstract
Background: Chimeric antigen receptor T cell (CART) therapy is revolutionizing modern cancer therapy, with two anti-CD19 CARTs FDA-approved for relapsed/refractory B cell lymphoma/leukemia and many other CARTs for solid and liquid tumors currently undergoing clinical trials. Our group recently demonstrated multiplexed CRISPR/Cas9 gene-editing of anti-CD7 CARTs to produce CD7 and T cell receptor alpha constant (TRAC)-deleted "off-the-shelf" universal (U)CART7s that effectively kill CD7+ T cell lymphoma in vivo without causing GVHD or fratricide (Cooper et al, Leukemia, 2018). However, in current clinical practice, suboptimal CART persistence and tumor killing permit tumor cell escape and, ultimately, disease relapse. Reasoning that a pro-lymphoid growth factor could promote CART efficacy, we supplemented UCART infusion with subcutaneous injections of the long-acting form of recombinant human interleukin-7 fused with hybrid Fc (rhIL-7-hyFc, NT-I7) in vivo using a CD19+ lymphoma xenograft model.
Methods: To create anti-CD19 universal CARTs (UCART19), we activated human T cells on CD3/CD28 beads, electroporated the T cells with Cas9 mRNA and a TRAC-targeted gRNA, and virally transduced an anti-CD19 scFv 3rd generation CAR containing a peptidase 2A-cleaved human CD34 construct for both purification and tracking in vivo. Residual TRAC+ cells were depleted using magnetic selection. For xenograft tumor modeling in vivo, we injected NOD-scid IL2Rgammanull (NSG) mice with 5x105 RamosCBR-GFP cells four days prior to UCART19 (2x106 cells). Mice were treated with NT-I7 (10mg/kg SC) on days +1, +15 and +29 post UCART19 infusion.
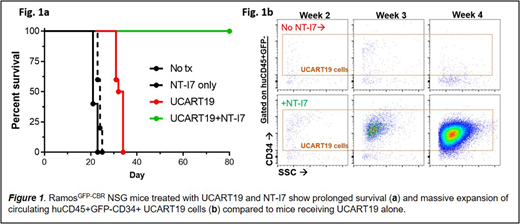
Results:RamosCBR-GFP mice receiving NT-I7 without UCART19 (NT-I7 only group) survived marginally longer (24 day med survival) than mice receiving RamosCBR-GFP cells alone (No tx group) (21 day medium survival, p=0.018, NT-I7 only vs. No Tx). While RamosCBR-GFP mice treated with UCART19 alone (UCART19 group) survived 33 days, 100% of RamosCBR-GFP mice treated with UCART19 and NT-I7 (UCART19+NT-I7 group) were alive at 80 days (Fig 1a), with no mouse showing signs of xenogeneic GVHD (p<0.0001, UCART19+NT-I7 vs. UCART19). At three weeks post UCART19 infusion, bioluminescent imaging (BLI) revealed minimal tumor signal in UCART19+NT-I7 treated mice (108 vs. 1010 photon flux/s, p<0.05, UCART19+NT-I7 vs. UCART19) and near-undetectable photon flux/s at four weeks (107 vs 1011 photon flux/s, p<0.0001, UCART19+NT-I7 vs. UCART19). Quantitative 17-parameter flow cytometric analyses of the blood, bone marrow, and spleens revealed an up to ~8000-fold increase in UCART19 cells in NT-I7-treated mice four weeks post UCART19 infusion (Fig 1a). These UCART19 cells demonstrated a predominantly effector and effector memory phenotype.
Discussion: CARTs engineered to express interleukin-7 and CCL19 showed increased migration to and killing of solid tumors (Adachi et al, Nature Biotechnology, 2018). However, genetically engineered potentiation strategies lack "off-switches" and may preclude additional genetic enhancements required for universal "off-the-shelf" CART development. Here, we demonstrate that a pharmacological grade long-acting interleukin-7 agonist can potentiate adoptive cellular therapies. Specifically, NT-I7 can dramatically enhance gene modified T cell proliferation, persistence and tumor killing in vivo, resulting in enhanced survival, providing a tunable clinic-ready adjuvant for reversing suboptimal CART activity in vivo.
Cooper:WUGEN: Consultancy, Equity Ownership. Lee:NeoImmuneTech: Employment. Park:NeoImmuneTech: Employment.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal